
Restorative & Therapeutic Treatments

Bite Adjustments
A bite is considered to be healthy when all or most of the teeth are present and not destroyed by normal daily usage.
It is destructive when teeth show wear, looseness or when TMJ (jaw joint) damage is seen. Bite therapy helps restore a bite that can function without damage and destruction. Multiple missing or damaged teeth interfere with your ability to chew properly and can lead to significant other problems such as jaw joint pain, over-stress to remaining teeth and even digestive problems.
Bite Adjustments
The therapy may include:
- Reshaping the biting surfaces of the teeth and eliminating spots of excessive pressures where the teeth are brought into contact. This is done by carefully dividing bite pressures evenly across all of the teeth.
- Bite splint therapy using a custom-fitted and adjusted plastic bite guard to keep the teeth apart, worn during the day, at night, or both.
- Braces to reposition mal-aligned or drifted teeth.
- Replacement of old, worn out, or damaged fillings.
- Reconstruction of badly worn and damaged teeth.
- Replacement of missing teeth with dental implants.
Bruxism Treatments
Bruxism is an oral parafunctional activity that commonly occurs in most people at some point in their lives.
The two main characteristics of this condition are grinding of the teeth or clenching of the jaw. These actions usually occur during a person’s sleeping hours, but may also occur during the day, particularly when stressed.
Bruxism is one of the most common known sleep disorders. The most common symptoms are earaches, headaches, muscle pain and tooth discomfort, but can lead to difficulty in eating or opening and closing your mouth.
Bruxism Treatments
Why should I seek treatment for Bruxism?
- Damage to teeth. Clenching and grinding can lead to tooth looseness and/or fracture. Broken teeth may require dental restoration or may need to be extracted if not restorable.
- Facial pain. Continual muscle contraction can lead to pain in the muscles of the head, neck and face, often presenting as headaches. More severe cases may experience difficulty opening or closing the jaw, or pain in the joint area during function.
- Occlusal trauma. The excessive wear on the occlusal (chewing) surfaces of the teeth from prolonged bruxing can not only damage individual teeth but may also alter the entire jaw relation and affect your ability to eat and speak, and even change your facial appearance.
- Arthritis. In the most severe cases, bruxism can eventually lead to painful arthritis in the temporomandibular (TMJ) joints that allow the jaw to open and close smoothly.
Treatment Options
Though there is no known cure for bruxism, there are a variety of devices and services available through our office to help treat bruxism:
- Mouthguards. An acrylic mouthguard can be designed from teeth impressions to minimize the abrasive grinding action during normal sleep. Mouthguards must be worn on a long-term basis to help prevent tooth damage.
- Soft Mouthguards. Soft, rubbery mouthguards, similar to an athletic mouthguard, can be fashioned if you clench your teeth and help protect your teeth from damage.
- TMJ/TMD Referral. We work with excellent dentists who focus their practices on TMJ issues and facial pain and refer to them for those cases beyond our level of care and expertise.

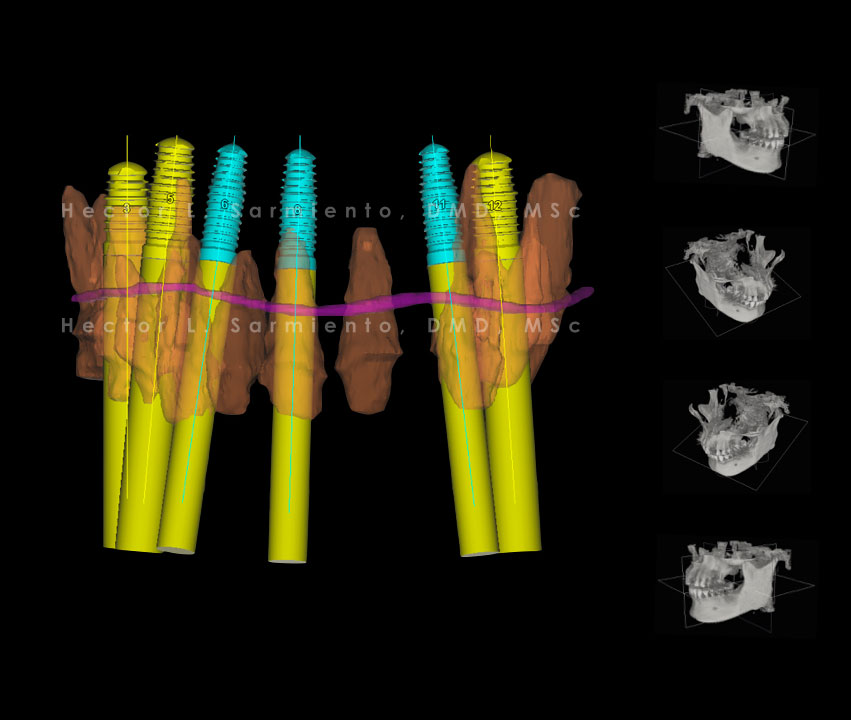
Computer Guided Surgery
As dental technology continues to advance, complicated procedures like dental implant surgery have become much more precise.
With the goal of always providing patients with the best surgical care possible, Dr. Hector L. Sarmiento, is proud to offer computer guided surgery. This advanced technology is utilized during dental implant surgery for patients with more complex needs. Through the state-of-the-art system, our team is able to more accurately place implants, as well as keep patients informed throughout the process.
For any questions or concerns regarding if this treatment is right for you, please contact our office to schedule you a consultation.
Dental Implants
A dental implant is a medical device commonly made from titanium and special additives to make its surface fuse to the jaw bone.
This process is called osseoinergration and occurs through a cascade of cells that approximates the bone to the implant. An implant (screw shaped) is surgically inserted in to the bone and needs an abutment which connects the implant to crown. The implant process can begin immediately after tooth extraction. In some cases, depending on the bone quality, additional healing time may be needed prior to implant placement. The surgical placement of an implant is fast, safe and requires minimal suturing. Healing of 2-6 months are needed depending on the site of the mouth prior to its restoration.
Dental Implants
Are dental implants safe?
Dental implants have a safe success rate of 97%. In some cases, your body may reject the implant and an additional surgery may be needed. The use of clinical and radiographic interpretation allows Dr. Sarmiento to see the anatomical structures of the head such as, sinuses and major nerves. Our office accommodates in house CT imagining to which provides a three dimensional view of your head to aid implant placement.
Am I a candidate for dental implants?
An overall good health status is required to be a candidate for dental implants. A medical consult between Dr. Sarmiento and your physician may be needed if you present any systemic disease or medications that can complicate a step in the surgical procedure. It is in Dr. Sarmiento’s best interest to keep you safe during your implant procedure.


Full Mouth Rehabilitation
A full mouth rehabilitation seeks to rebuild every tooth in the mouth and requires highly educated and qualified dental specialists.
The results are amazing. Dr. Hector Sarmiento and his team can create the perfect smile according to your facial proportions. Dr. Sarmiento is very well trained and qualified in the field of cosmetic surgical dentistry.
The case shown here is a satisfied patient that was co-treated by Dr. Sarmiento and Dr. Llobell (Spain) to achieve maximum esthetics. The rehabilitation included multiple dental implants to replace the patient’s hopeless teeth and fixed prosthesis were designed to give her a beautiful natural look.
Laser Periodontics
Lasers can be used in gum surgeries, as well as to treat infections in dental implants.
Dr. Hector Sarmiento is fully trained in lasers. He lectures other dental specialist in the clinical use of lasers. In periodontics lasers are used to make procedures less invasive by minimizing patient discomfort and avoiding trauma to the gums.
Laser Periodontics
Lasers To Treat Infected Dental Implants
Dr. Sarmiento uses laser therapy to decontaminate infected dental implants. He has worked extensively in infected implant (periimplantitis) research using lasers as part of the treatment approach.
Laser Gum Surgery
Although lasers have not been proven scientifically to show better results over conventional therapies, Lasers are used to create a pain free environment. In some cases, the laser may be used to reduce gum diseases and avoid a surgical procedure. Research from the American Academy of Periodontology suggests that using lasers as an adjunct to scaling and root planing (SRP) may improve the effectiveness of this procedure. In addition, when lasers are used properly during periodontal therapy, the patient experiences less bleeding, swelling and discomfort during surgery.
Cold Sore Treatment NYC
Dr. Hector Sarmiento provides laser treatment for cold sores and canker sores. By using a laser,Dr. Sarmiento can more effectively treat cold sores and canker sores. Usually cold sores remain in the mouth for 2 weeks and are painful. With laser removal, the sores can be fully eliminated in 2-3 days, promoting faster healing and prevents them from spreading to other parts of the mouth. If you notice signs of a cold sore, such as a tingling, itching, or painful feeling around your mouth and lips, schedule an appointment for a laser treatment as soon as possible.
Laser Gum Discoloration Treatment
A natural reason that a person may have darker gums that are black or dark brown is skin pigmentation balance. Just as skin color can vary, so can gum color. For some people, often of non-Caucasian descent, gums can have spotted darkness or may not be pink at all. Patients with discolored gums have the option to whiten (pink) with a non invasive procedure using lasers. Depending on the amount of discoloration or how dark the gums are, a single or multiple procedures may be necessary.
Dental lasers can be used to:
- Reduce the discomfort of canker and cold sores.
- Expose partially erupted wisdom teeth.
- Remove muscle attachments that limit proper tongue or lip movement.
- Remove overgrown tissues caused by certain medications.
- Perform biopsy procedures.
- Remove inflamed gum tissues and aid in the treatment of gum disease.
- Remove or reshape gum and bone tissues during crown lengthening procedures.
- Speed up tooth whitening procedures.
- Remove black gums.
- Treat infected dental implants.
Be aware that at this time, there is insufficient evidence to suggest that any specific laser wavelength is superior to the traditional treatment methods of the common periodontal diseases, such as periodontitis.


Periodontal Maintenance
After Dr. Pollack, Odrich or Sarmiento has completed the active phase of periodontal treatment, he will provide you with a personalized maintenance program of care to keep your gums healthy.
Supportive periodontal therapy is an ongoing program designed to prevent recurrent disease in the gum tissues and bone supporting your teeth. Adherence to a program of conscientious oral home care and regularly scheduled maintenance therapy visits with your dentist and Drs. Pollack, Odrich or Sarmiento will give you the best chance of keeping your teeth and gums healthy and looking and functioning their best. Periodontal maintenance treatment incorporates what you’re probably used to getting during a regular dental prophylaxis treatment at your dentist, but also does more, to treat and maintain good periodontal health.
Periodontal Maintenance
Why is supportive periodontal care important?
As you have learned, you are susceptible to gum disease. And, you have probably learned, too, that the main cause of gum disease is bacterial plaque, a sticky, colorless film that constantly forms on your teeth. The bacteria in this plaque produce toxins, or poisons, which constantly attack your gums and teeth. Unless plaque is removed, it hardens into a rough, porous deposit called calculus, or tartar. Daily brushing and flossing will help to minimize the formation of calculus, but it won’t completely prevent it. No matter how careful you are in cleaning your teeth and gums, bacterial plaque can cause a recurrence of gum disease from two to four months after your last professional cleaning. Therefore, a dental professional must check for hidden problems and remove the hardened plaque at time intervals appropriate for you so that your teeth and gums stay healthy.
Who should perform supportive periodontal therapy?
The answer depends on you and the severity of your gum disease. Generally, the more severe your periodontal disease initially, the more often Drs. Pollack, Odrich and Sarmiento will need to oversee your care. Together, you, your general dentist and Drs. Pollack, Odrich or Sarmiento will work out the most effective schedule for your supportive periodontal care.
Your maintenance/supportive periodontal care visit may include:
- discussion of any changes in your health history
- discussion of any dental problems or concerns you’ve noted
- examination of your mouth tissues for abnormal changes
- measurement of the depth of pockets around your teeth
- determination of any mobility of your teeth and possible causes
- assessment of your oral hygiene habits and provision of instruction
- removal of bacterial plaque and tartar
- polishing, or prophylaxis, to remove stain and brighten your teeth
- periodic x-rays to evaluate your teeth and bone
- examination of your teeth for decay and other dental problems
- checkup on the way your teeth fit together when you bite
- application or prescription of medications to reduce tooth sensitivity or other problems you may have.
How often should you have supportive periodontal care visits?
Your periodontal condition is the deciding factor. The interval between your supportive periodontal care visits might be as often as every few weeks or as frequent as every six months. Everyone’s situation is different. The frequency of your supportive care visits will be influenced by:
- the type of periodontal disease you have
- the type of periodontal treatment you’ve had
- your response to treatment
- your susceptibility to further breakdown
- your rate of plaque growth
- your commitment to good oral home care
What is the relationship between your dentist and Drs. Pollack, Odrich and Sarmiento?
Your dentist and Drs. Pollack, Odrich and Sarmiento work together as a team to provide you with the best possible care. They combine their experience to formulate the best maintenance plan for you. They keep each other informed about your progress. Although Drs. Pollack, Odrich or Sarmiento may see you periodically for maintenance therapy, you will need to see your general dentist as well. Appointments for periodontal maintenance do not replace regular dental checkups. If Dr. Pollack, Odrich or Sarmiento detect tooth decay during a maintenance visit, he will refer you to your general dentist for treatment. Your general dentist is primarily responsible for your overall dental health, including such dental needs as filling new or recurrent cavities or making changes in fillings, crowns or bridges.
To prevent periodontal disease, the major cause of tooth loss in adults—and keep your natural teeth healthy—carefully and conscientiously follow the guidelines of the maintenance program that Dr. Pollack, Odrich or Sarmiento recommends. Protecting your periodontal health through preventive maintenance has great benefits for you. You will be able to chew with more comfort, and you will be able to smile and speak with greater confidence. You will be able to keep dental costs down by preventing future problems. Your commitment to maintenance therapy is your commitment to your better oral health.
Periimplantitis
What causes periimplantitis?
The main cause of periimplantitis is bacteria. The lack of brushing or flossing of the dental implant is the main risk factor. Others include smoking, stress, previous periodontal diseases, infected neighboring teeth, suboptimal surgical or prosthetic execution, and/or improper maintenance care. Dr. Hector Sarmiento is one of the few periodontist in the nation who is treats periimplantitis. He has created methods to decontaminate the dental implant with a variety of special instruments and lasers, ultimately allowing a bone graft to be placed and save the implant. To help others minimize and thoroughly understand the disease, Dr. Sarmiento finds great pleasure in lecturing and teaching his techniques to other Specialists. The case above is one of many treated by Dr. Sarmiento that has resulted in success at a 3-year evaluation. This patient was told by his dentist he had to remove the infected implant and that he may lose more bone thereafter. This would have concluded in a non-esthetic result and could have caused an undesirable environment for future placement of a second implant. Due to Dr. Sarmiento’s minimally invasive and conservative approach which is the hallmark of his treatments, he was able to avoid any unwanted results.
Periimplantitis
How can I prevent periimplantitis?
Dr. Hector Sarmiento recommends after you have your dental implant placed in your mouth, visit your periodontist every 3-6 months for implant maintenance and avoid the risk of a disease developing. Periimplantitis may still develop but can be diagnosed at an earlier stage, allowing us to treat it without a surgical procedure. Dr. Sarmiento’s office is known as the Center for Treatment and Prevention of Periimplant Diseases.

Scaling and Root Planing
The initial stage of treatment for periodontal disease is usually a thorough, deep cleaning, scaling and root planing, or SRP.
The objective of these non-surgical procedures is to remove etiologic agents such as dental plaque and tartar, or calculus, which cause gingival inflammation and disease. Scaling and root planing removes bacterial deposits on the root surfaces under the gums, allowing the gums to heal. SRP may be your only treatment for cases of gingivitis and early periodontitis, but is also included in treatment for more severe disease.
Scaling and Root Planing
What do the procedures entail?
Drs. Pollack, Odrich or Sarmiento will only perform scaling and root planing after a thorough examination of the mouth, which may include taking x-rays and visually examining the mouth. Depending on the condition of the gums, the amount of tartar present, the depth of the pockets, and the progression of periodontitis, Drs. Pollack, Odrich or Sarmiento may recommend scaling and root planing. In some cases, local anesthesia may be used during the procedure, although very often only topical anesthetic creams are necessary.
- Scaling:
When scaling is performed, calculus and plaque that attaches to the tooth surfaces is removed. The process especially targets the area below the gum line, along the root. Scaling may be performed with a special dental tool called an ultrasonic scaler, or cavitron, but is usually also completed with hand scaling with specially designed instruments to reach below the gum line without damaging the gums. - Root Planing:
Root planing is performed in order to remove cementum and surface dentin that is embedded with unwanted microorganisms, toxins and tartar. The root of the tooth is literally smoothed, which promotes healing, and also helps prevent bacteria from easily colonizing in the future. - Antibiotics or irrigation with anti-microbials (chemical agents or mouth rinses) may be recommended to help control the growth of bacteria that create toxins and cause periodontitis. In some cases, Drs. Pollack, Odrich or Sarmiento may place antibiotic fibers in the periodontal pockets after scaling and planing. This may be done to control infection and to encourage normal healing.
- When deep pockets between teeth and gums are present, it is difficult to thoroughly remove plaque and tartar. Patients can seldom, if ever, keep these pockets clean and free of plaque. Consequently, surgery may be needed to restore periodontal health.
Benefits of Treatment
- If treatment is successful, scaling and root planing may have many periodontal benefits. One is that it can help prevent disease. Research has proven that bacteria from periodontal infections can travel through the blood stream and affect other areas of the body, sometimes causing heart and respiratory diseases. Scaling and root planing remove bacteria that cause these conditions.
- Another benefit of treatment is protecting teeth against tooth loss. When gum pockets exceed 3mm in depth, the risk for worsening periodontal disease increases. As pockets deepen, more bacteria are able to colonize, eventually causing a chronic inflammatory response by the body to destroy gingival and bone tissue. This leads to tooth loss. SRP often allows the gums to heal, causing pockets to shrink and become more readily maintained.
- Finally, scaling and root planing may make the mouth more aesthetically pleasing, and should reduce bad breath caused from food particles and bacteria in the oral cavity. Superficial stains on the teeth may also be removed during scaling and planing, adding an extra bonus to the procedures.
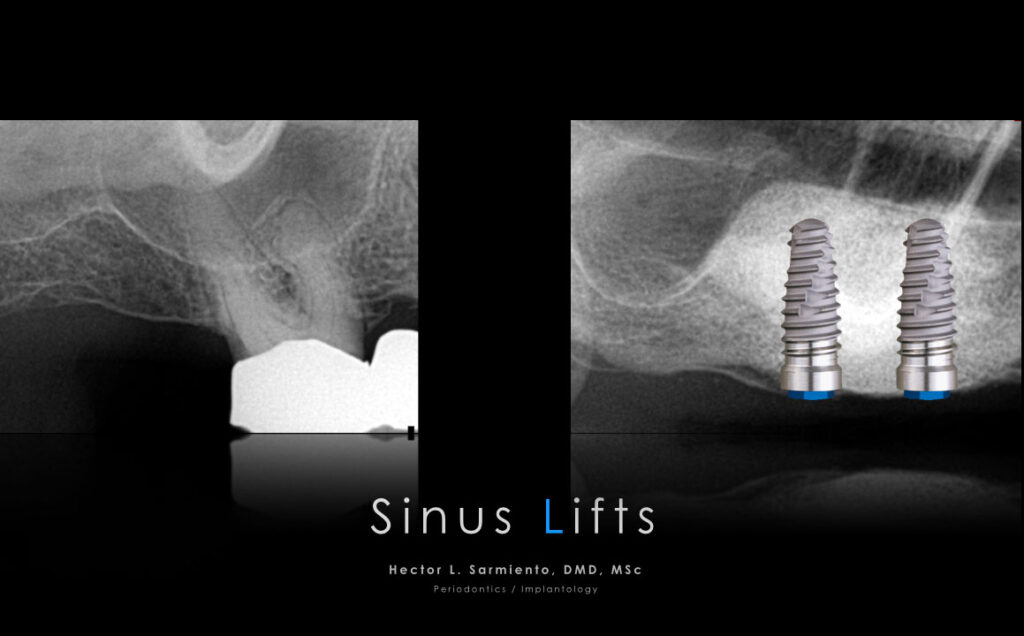
Sinus Lift
A sinus lift is surgery that adds bone to your upper jaw in the area of your molars and premolars. It’s sometimes called a sinus augmentation. The bone is added between your jaw and the maxillary sinuses, which are on either side of your nose.
The X-rays above show a tooth that is piercing through the sinus floor (left). In order to place dental implants in this area, a sinus lift surgery is need to create space and allow the implants to fit properly. On the right X-ray, a successful sinus augmentation was performed, creating enough space for two implants.
For any questions or concerns regarding if this treatment is right for you, please contact our office to schedule you a consultation.

Soft Tissue and Bone Grafts
Receded Gums
The case above shows the initial situation of gums that have receded. The arrows indicate where the gum tissue should be. After a conservative tissue graft surgery the gums are in the appropriate area. The final picture is after 4 years.
Bone Grafts
Often due to advanced periodontal diseases, the bone and surrounding tissues disappear and need to be regenerated through bone grafting.
For any questions or concerns regarding if this treatment is right for you, please contact our office to schedule you a consultation.

